Insulin is a hormone produced by the pancreas and it helps the muscles and organs take up the blood sugar that is needed to function properly.
With Diabetes mellitus, the blood sugar level is raised because of a lack of insulin.
Diabetes varies markedly in different ethnic groups and there is a high prevalence in Asiatic people and urban dwellers. 1% of pregnant women under the age of 35 will have diabetes or impaired glucose tolerance.
Due to advances in medicine, most diabetic women have perfectly healthy babies. The key to a safe pregnancy is pre-conceptual planning and tight control of blood sugar levels. These levels change significantly throughout pregnancy.

Insulin-dependent diabetes is diagnosed during childhood and sufferrers need insulin injections daily.

Non-insulin dependent diabetes is more common in older people (>40 years) and who are overweight. Diet and medication control this type of diabetes.

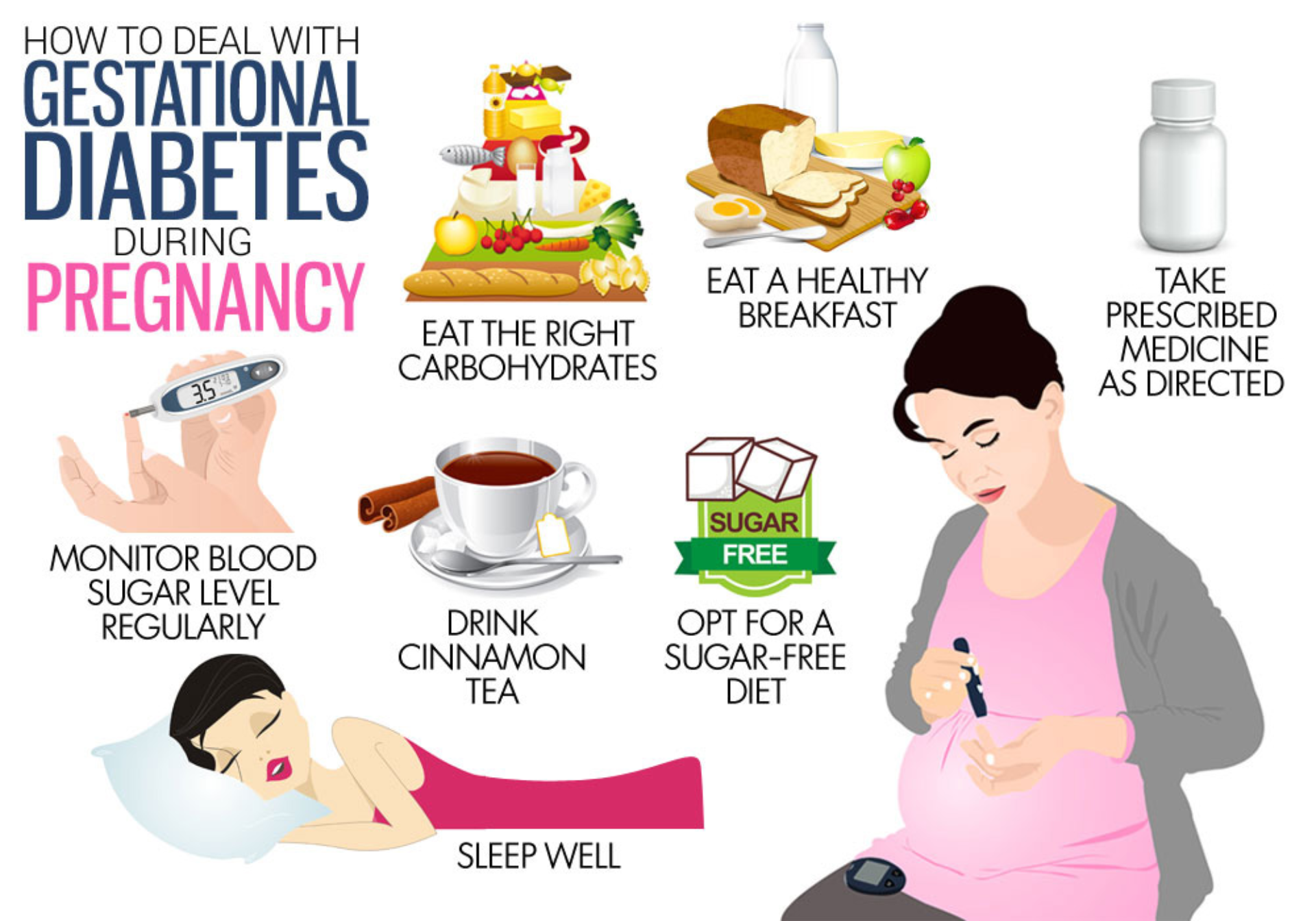
Gestational diabetes develops during pregnancy and may persist after the birth.
Gestational Diabetes develops during pregnancy and may persist after the birth. Due to advances in medicine, most diabetic women have healthy babies.
If you are planning a baby, but were diagnosed with diabetes, you may have special health concerns. The pregnancy will affect your blood sugar levels and diabetes medications.
The medical practitioner may also test or assess the following:
Many women don’t know they’re pregnant until the baby has been growing for 2 to 4 weeks. That’s why you should have good control of your blood sugar before you start trying to conceive.
Keep blood glucose levels within the ideal range:
High blood sugar levels early in the pregnancy (before 13 weeks) can cause birth defects. They also can increase the risks of miscarriage and diabetes-related complications.
From the 10th week of pregnancy your blood glucose lowers because of the increased levels of estrogen and progesterone in blood. These pregnancy hormones stimulate the production of insulin.
From the second trimester, all pregnancy hormones increase, especially the placental hormones; this leads to an increased resistance to insulin. For this reason, insulin is less effective in regulating blood glucose, especially at night.
If you use insulin to control your diabetes, your doctor can tell you how to adjust your dose. Your body will probably need more while you’re pregnant, especially during the last 3 months.
Labour can be a stressful time for you and the baby. If you’ve been using insulin during your pregnancy, insulin needs will continue through labour. It’s typically continued with an IV or with a pump if you are already on a pump. Right after delivery, your need for insulin will likely drop quickly.
Gestational diabetes means that the diabetic condition developed in pregnancy because the pancreas could not meet the increased need for the blood-glucose regulating hormone insulin. This result in poorly controlled blood glucose levels because insulin is not being made in enough amounts.
When gestational diabetes develops, the pregnancy will be regarded as “high-risk” because the risk for developing hypertension (high blood pressure), blood clots, kidney disease and diabetic retinopathy [eye problems] increases.

Every pregnant woman should be tested for diabetes mellitus during their first antenatal visit and again between 16-28 weeks of gestation to identify those women at risk.

Because of the risks for you and your baby, antenatal care is essential. You should go for a consultation as soon as you suspect a pregnancy. If you are a known diabetic or has a BMI of more than 35, you need to consult with the medical practitioner before you conceives. Birth defects can substantially be minimized by proper control of blood sugar levels.
Women with well controlled diabetes often go full-term without any problems. However, many doctors prefer to plan for an early delivery, usually around weeks 38-39.


Diana du Plessis is an independent Midwifery consultant and researcher. She specializes in midwifery and neonatology and lectures widely to nursing professionals and academic audiences on a national and international level.
She is a passionate childbirth educator and national spokesperson on breastfeeding. She is the author and co-author of various nursing and midwifery publications (books and peer-reviewed articles).